COVID-19 in Uganda
OCTOBER 20, 2020
COVID-19 HAS REACHED LACOR HOSPITAL
It was inevitable. Uganda resisted an outbreak as long as possible, having a significantly lower number of positive cases than neighboring countries. But COVID-19 has crossed the gates of Lacor Hospital despite the protective measures that have been in place since last February. Until recently, there were only suspected cases at Lacor. When cases were confirmed, the Ugandan Ministry of Health transferred infected patients to a nearby governmental hospital, leaving Lacor to continue maintaining everyday healthcare for patients in the community.
The first person who died from COVID-19 at Lacor was a hospital driver; we will call him Oceng Robert. About ten days ago, he arrived at the hospital feeling ill. He was coughing, struggling to breathe, and suffering from hypertension. Health workers immediately transferred him to the Intensive Care Unit (ICU), where he was attended to by the nurses, while his wife and son stood by.
Oceng passed away the day after his arrival; nothing could have been done to save him.
“Everyone who came in contact with him was tested,” assures nurse Janet Adong, head of the Covid-19 ICU, “and the tests all came back negative.”
WHAT DOES COVID-19 LOOK LIKE IN UGANDA?
On September 24th, the number of confirmed cases in Uganda was 7064, with 70 deaths. On average, between 2,000 and 3,000 tests are administered daily, with 200 patients testing positive each day.
Last Sunday, President Museveni spoke to the nation regarding the renewal of some restrictive measures and the relaxation of others.
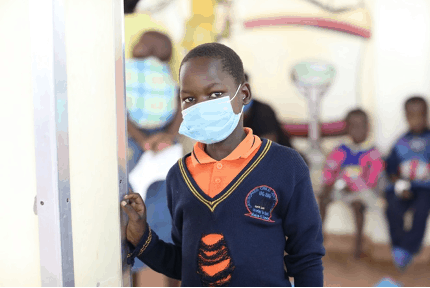
Schools are currently closed. A curfew will continue from 9 p.m. to 6 a.m. However, boda bodas, the local form of transportation, must stop running at 6 p.m. This is problematic because people depend on boda bodas to travel long distances and in emergencies.
In the Gulu area, where the hospital is located, 733 positive cases have been recorded, 428 of which have been hospitalized. The high number of hospitalizations seems to mask more infections than are diagnosed.
AMONG THE STAFF AT LACOR, EIGHT PEOPLE HAVE TESTED POSITIVE.
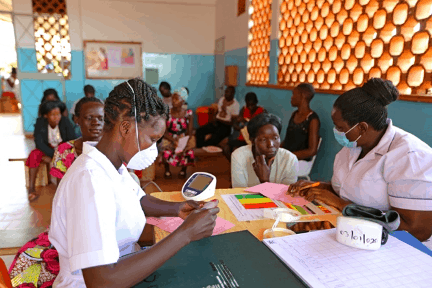
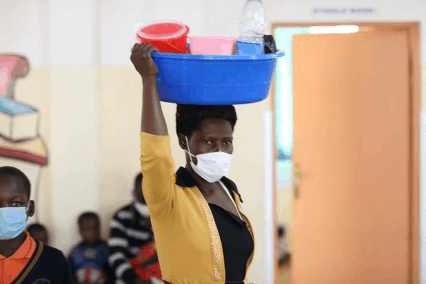
Hospital staff remains alert, ready to welcome the most serious patients as well as those that the now saturated government hospital cannot handle.
“The limited number of spaces remaining at Gulu Regional Referral Hospital is the current challenge,” said Dr. Alfred Okello, Lacor’s Public Health specialist. “Our staff is diligent about observing precautions such as wearing masks and washing hands. However, maintaining social distance is still a problem,” he confides.
The hospital has faced numerous epidemics throughout its history: from HIV to meningitis to Ebola. Now, it faces COVID-19.
“If you are convinced of what you are doing and if you really believe in it, then you stay,” Lucille Teasdale, founder of the hospital declared to those who asked her to leave the hospital in the darkest years of the civil war.
Strengthened by your support, the hospital staff, too, remains steadfast and look towards the future.